| Treatment Options |
Lumpectomy |
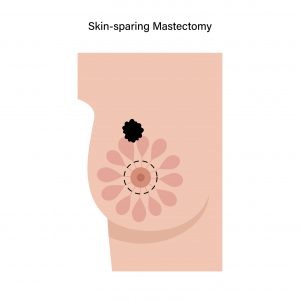
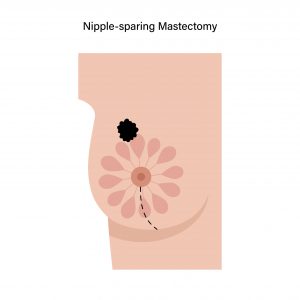
Mastectomy |
Mastectomy with Reconstruction Surgery |
Who is suitable for the procedure?
|
Who is suitable for the procedure?
- Cancer only affects a portion of the breasts.
- The tumour is relatively small compared to the breast.
- The patient is medically fit to undergo surgery and follow-up radiation therapy.
|
Most patients can also opt for mastectomy if:
- Cancer affects more than one area of the breast.
- The tumour is relatively large compared to the breast.
- The patient is not fit to receive radiation therapy.
- Patient’s choice to undergo a mastectomy.
|
Patients who decided for mastectomy can choose to undergo reconstruction surgery if they wish to. |
What are the risks?
|
You may feel fatigued, or experience skin changes from the radiation treatment. |
You may feel imbalanced, especially if you had large breasts. This may lead to neck or shoulder aches. |
You may be dissatisfied with how your new breasts look. In the case of your implants, they may:
- Break or leak, requiring additional surgeries.
- Harden, causing pain.
|
|
Other possible complications may include: |
|
- Formation of scars
- Bleeding
|
|
|
Will insurance cover the surgery expenses?
|
Every insurance plan is different. You should check with your insurance company to determine whether your plan covers the surgery costs. Visit our billing & payment page to find out which are the insurance providers we collaborate with. |
How long will I take to recover?
|
3 – 4 weeks |
3 – 4 weeks |
6 – 8 weeks
However, depending on the type of reconstruction done, it may take longer to recover. |
|
Note: Recovery time differs for each patient, depending on the severity of cancer and the extent of surgery. |
What additional treatments will I need?
|
Radiation therapy is usually done within a few weeks after lumpectomy. |
Radiation therapy may be required depending on the situation, and extent of the disease |
|
Depending on your condition, other types of treatment may include: |
|
- Hormone therapy
- Chemotherapy
|
|
What will my breasts look like after surgery?
|
Your breast should be very similar to what it looked like before surgery.
However, depending on the size of the lump, your breast may look smaller. |
You will have a flat chest on the side where your breast was removed. |
You will have a breast-like shape, but it will not look like it did before surgery. |
|
You will also have scars at the surgical site. |
Scars will form at the site where the skin is stitched to create a new breast-like shape. |
Will my breasts have any feeling after surgery?
|
Yes, you should still have feeling in most parts of your breasts, however there may be numbness over the site of the surgery or your armpit. |
Depends. The surgical site may have a numb feeling. This numbness may disappear after 1 or 2 years but will not feel the same as before surgery. |
No. The area around your breast will not have any feeling. |
What are the chances of breast cancer recurrence?
|
The chance of the cancer coming back is similar whether a patient undergoes a Lumpectomy (Breast Conserving Surgery (BCS)) or mastectomy. |